Putting Equity at the Center of Childhood Injury Prevention
Children in the U.S. die from injury at drastically unequal rates, with children who identify as Black, American Indian, rural, or lower income at highest risk. Identifying solutions to systematically address these inequities is paramount in making sure all children can access their human right of health and safety.
Injuries – including unintentional ones such as car crashes, and intentional ones, such as violence and self harm – are the leading causes of death in U.S. children over the age of 1, leading to more deaths than heart disease, cancer and influenza combined. Significant inequities exist in who is injured by race, geographic location and socioeconomic status:

Black children die from injury at
4.5 times the rate of Asian American children and 2 times the rate of white children.

American Indian children die from
injuries at 3.5 times the rate of Asian American children and 1.4 times the rate of white children.

Children in rural communities
die from injuries at 2 times the rate of children in urban communities, with risk from multiple injury mechanisms.
A Framework for Understanding the Cause of Inequities
While injury prevention strategies have improved over the last decade and the prevalence of many injuries has decreased, inequities have persisted. We developed the Injury Equity Framework to analyze inequities in childhood injuries resulting in death or serious injury, and to better understand how to address them systematically. The Injury Equity Matrix was developed as a companion tool.

The Injury Equity Framework provides a conceptual foundation to understand the complex multilevel factors which contribute to injury inequities. The framework is grounded in societal factors through which discrimination and stigma have operated historically and continue to operate today. These factors include ableism, classism, racism, sexism, homophobia, transphobia, and xenophobia, all of which operate at structural and individual levels. We'll review components of the framework, starting with intersectionality on the left. Intersectionality refers to the complex social identities which distinguish an individual or group, and include community, family, and individual factors. The intersectionality of an individual or group, within the context of societal factors, puts some individuals and/or groups at higher risk for an injury to occur, and for increased injury severity or and/or death.
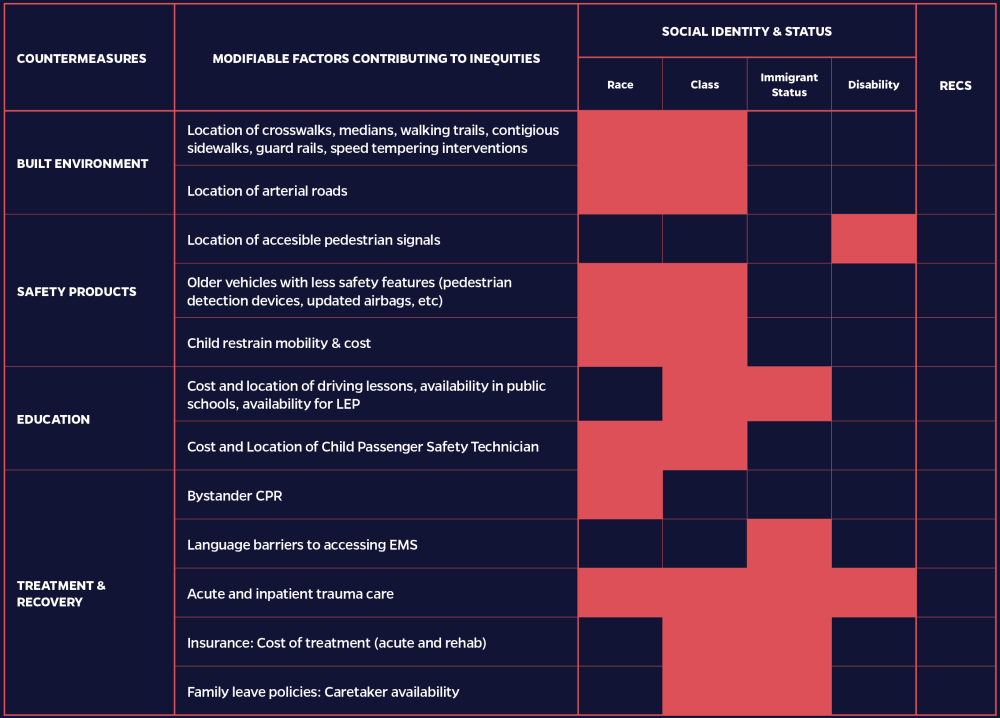
The phases of injury are based on the Haddon Matrix, which is regularly used to describe factors that impact injury outcomes, and five major injury countermeasures distributed among the phases where they are most active. We created the Injury Equity Matrix as a companion working tool to the Injury Equity Framework to help teams develop effective interventions to better address injury inequities (available in the downloadable toolkit).
The Nation’s First Pediatric Injury Equity Review
We established the Massachusetts Pediatric Injury Equity Review (MassPIER) – a new process for reviewing inequities in injuries and identifying recommendations with experts in injury surveillance, child fatality review and legislative advocacy.
Partners:
- The Boston Medical Center (BMC) Department of Pediatrics (Project Lead)
- Johns Hopkins Center for Injury Research and Policy (Evaluation Partner)
- Massachusetts Department of Public Health (Data Collaborator)
- Suffolk, Middlesex, & Norfolk County District Attorney’s Office Child Fatality Review Teams (Collaborator)
We implemented the MassPIER review process, as described below with the Middlesex County Child Fatality Review Team to find equity-based solutions.
Reviewed Case & Epidemiologic Data
As a team, we discussed specific traffic injury case fatalities, and identified similarities and themes.
We reviewed epidemiologic data provided by the Massachusetts Department of Public Health for Middlesex County and Massachusetts from 2016-2020, and found:
- Fatal pedestrian and motor vehicle occupant injuries were low at the county level and thus difficult to evaluate for inequities.
- There were significant racial inequities in emergency department visit rates for non-fatal pedestrian injuries in Middlesex County. Compared to white, non-Hispanic patients, the rate of emergency department visits for non-fatal pedestrian injuries were 3.4 times in Black, non-Hispanic patients and 2 times in Hispanic patients.
- Emergency department visits in Middlesex County for non-fatal motor vehicle occupant injuries had similar racial inequities, with rates 3 times higher for Black, non-Hispanic patients and 1.5 times higher for Hispanic patients, compared to white, non-Hispanic patients.
Reviewed GIS Mapping Data
We reviewed publicly available GIS mapping data to review location of fatal injuries. The blue icons represent fatal pedestrian injuries, helping to identify specific locations which may be hotspots for serious pedestrian crashes.
Developed Data-Driven Recommendations
As a team we discussed and developed recommendations to address the contributing factors to traffic injury. An example of preliminary recommendations identified during the team meeting included:
- Identifying the availability of free driver’s education and education in languages besides English with advocacy to increase access, if needed.
- Increasing the availability of free multilingual CPR training in communities of color.
- Making first-time intoxicated driving offenders eligible for ignition interlocks.
After the meeting, the Boston Medical Center team reviewed the recommendations and gave each recommendation an equity score and worked to identify priority areas and associated legislation, policy or programming and a plan for implementation. Recommendations were refined for dissemination and implementation in an ongoing process through iterative discussions with stakeholders and research into the policy landscape before being elevated to the State Child Fatality Review Team.
Save children’s lives in your community by implementing this process to identify solutions.
We established the Massachusetts Pediatric Injury Equity Review (MassPIER) – a new process for reviewing inequities in injuries and identifying recommendations with experts in injury surveillance, child fatality review and legislative advocacy.
The MassPIER process was created to be sustainable and scalable. We created a toolkit to assist anyone who wants to develop a Pediatric Injury Equity Review in their area.
Research Partners
This project was made possible through the support of the Bloomberg American Health Initiative and involved collaboration between experts and researchers, including:
Principal Investigator
Advisor
Research Coordinator
Research Assistant
Advisor
Advisor
Director of Injury Prevention & Control
Injury Prevention Policy Coordinator
Epidemiologist, Injury Surveillance Program
Child Fatality Review Epidemiologist
Suffolk County District Attorney's Office (Lead)
Norfolk County District Attorney's Office (Lead)
Middlesex County District Attorney's Office (Lead)
Suffolk County District Attorney's Office (Coordinator)
Norfolk County District Attorney's Office (Coordinator)
Middlesex County District Attorney's Office (Coordinator)